
Temporomandibular disorder is a group of diseases that affect the temporomandibular joint, masticatory muscles and other adjacent structures.
How can I recognize temporomandibular disorder?
The most common symptoms of these diseases include:
- pain in the temporomandibular joints,
- pain in the muscles of mastication,
- limited mandibular movements or deviations during abduction,
- sounds during mandibular movements, such as clicks or crepitations
What is the anatomy of the temporomandibular joint?
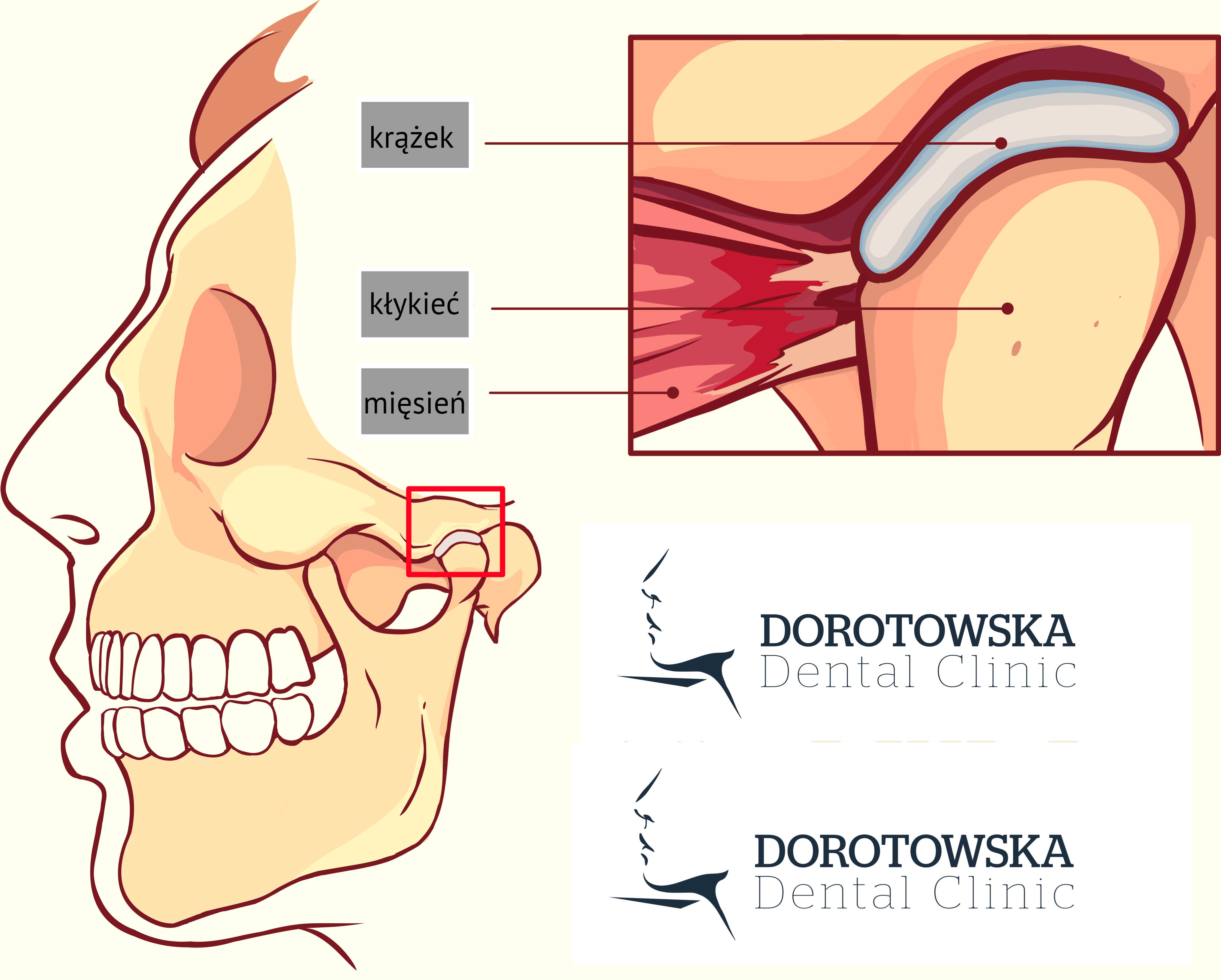
The mandible is a bone of the skull, which is not tightly connected by means of sutures to the remaining cranium, but it helps form structures that aid in the movements necessary to speak, eat and breathe. These structures are the two temporomandibular joints, the action of which is closely interconnected. They lie anterior to the external auditory meatus and are composed of the mandibular condyles (joint heads), and the articular surfaces of the temporal bones, in which we distinguish the articular eminence and the articular socket. These are basic bone structures, but the proper functioning of the joint is possible due to the presence of the following elements made of connective tissue:
- the articular disc - it divides the joint cavity into two parts, in which specific movements of the condylar heads take place, and the proper functioning of the joint depends largely on its position,
- the ligaments - a group of fibrous structures whose task is to strengthen the whole joint structure and to limit the slow movements of the mandible at the appropriate level.
The functions of the mandible are to aid any movements that can occur in the joints, triggered by the action of masticatory muscles:
- abduction (or lowering) and adduction (i.e. lifting) of the mandible,
- protrusion and retrusion
- lateral movements - constitute a synchronized combination of the above movements.
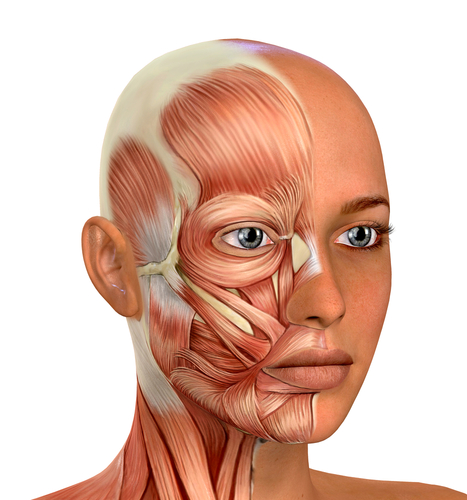
The muscles that enable these movements are the masticatory muscles. This group includes:
- the masseter muscles,
- the temporal muscles,
- the medial pterygoid muscles,
- the lateral pterygoid muscles – upper and lower heads
One should be aware that the described bone and muscle system is under strict control of the nervous system. There are a number of receptors and efferent fibers whose role is maintaining the mandible in the resting position, reacting to noxious stimuli, and performing intentional and conscious movements. It is a complex system of mutual dependencies in which damage to one element affects the entire system.
Why do I have temporomandibular disorder?
The origin of the described disorders has been a research problem for decades, which still remains unresolved. During the course of almost a whole century, a number of hypotheses have been put forward explaining their etiology. Possibilities include joint structure, disturbed muscle function, incorrect occlusion or mental factors. None of these theories have been completely confirmed, and the main conclusion is that temporomandibular disorder is a complex problem that may have multiple causes.
What does the diagnosis process look like?
In order to implement the appropriate treatment for a specific disorder, a detailed examination should be performed. After the interview and functional examination, sometimes supplemented with imaging examinations, the doctor can diagnose one of three main groups of disorders:
- pain in the muscles and the temporomandibular joints;
- internal disorders in the joint (most often dislocations of the articular disc);
- degenerative changes in the joint.
Each of these three main groups is characterized by a different therapeutic approach, and among them there are specific diseases that require specific actions.
What does the treatment process look like?
In a simplified way, the treatment of temporomandibular disorders includes the following basic steps:
- The elimination of pain - this is an extremely important stage of treatment, because pain is the most common reason for the patient to seek to a specialist in the field of temporomandibular disorders. Depending on the cause, this treatment may include muscle relaxation, pharmacotherapy and the use of occlusal splints.
- The next stage is an attempt to eliminate the original cause of the disorder. Depending on the etiology of the disorder in a given patient, the triggering factors may be:
- Occlusal abnormalities, i.e. the contact of opposing teeth - static and dynamic. In this case, the doctor thoroughly analyzes the existing conditions in the mouth and sets up a treatment plan including orthodontic or prosthetic corrections in order to obtain optimal occlusion,
- Abnormal muscle function - in this case the doctor makes a muscle relaxation device, i.e. a stabilization splint, and instructs the patient to perform a series of activities and exercises to relax and optimize the function of the masticatory muscles.
- Abnormal mandibular position in relation to the maxilla - this is a problem that requires a multi-stage approach. The first step is to determine the correct mandibular position, that enables synchronized work in the temporomandibular joints, and the second, is to fix it by recreating the correct occlusion. In the first stage, repositioning splints that reversibly alter the position of the mandible can be used, while the second stage is implemented through carefully planned orthodontic, prosthetic or other similar treatment.
- The mental factor - because of the high pace of life, nowadays stress is the main factor conducive to the development of temporomandibular disorders. High emotional stress causes the increased tension of masticatory muscles, which, in turn may cause pain. The long duration and persistence of pain can lead to the phenomenon of referred pain (felt in a different place than the source of pain) and back to the deterioration of the mental state of the patient (chronic pain). This pain may limit the patient in performing daily home activities, going to work, and contact with the environment. In these cases, in addition to good dental care, psychological and psychiatric support is needed, and sometimes cooperation with a chronic pain counseling center. Therefore, it is important to quickly eliminate pain (the first stage of treatment) so as to avoid the progression of the disease into a chronic form.
Offer
Warszawa Ochota
Adres:
ul. Dorotowska 9
02-347 Warszawa
Telefon: +48 501 328 772
E-mail: recepcja@ddclinic.pl
Godziny otwarcia:
Poniedziałek - Piątek: 9:00 - 20:00
Sobota: nieczynne
Warszawa Ursynów
Adres:
ul. Migdałowa 10 lok.5
02-796 Warszawa
Telefon: +48 502 070 050
E-mail: recepcjaursynow@ddclinic.pl
Godziny otwarcia:
Poniedziałek - Piątek: 12:00 - 20:00
Sobota: nieczynne
